26 Sep 2023
Disruptions between memory and appetite linked to obesity
BY Tom Walker
Disruptions in the way the human brain links memory and appetite could help explain some disorders associated with obesity.
Research from the Perelman School of Medicine at the University of Pennsylvania, US, suggests that disrupted connections between memory and appetite-regulating brain circuits are directly proportional to body mass index (BMI).
The link is most notable in patients who suffer from disordered overeating that can lead to obesity, such as binge eating disorder (BED).
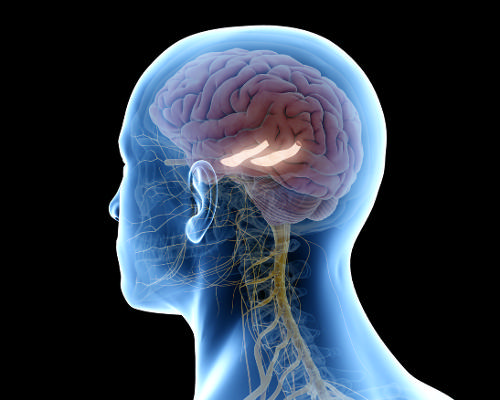
Published in the journal, Nature, the research – titled An orexigenic subnetwork within the human hippocampus – found that individuals who are obese have impaired connections between the dorsolateral hippocampus (dlHPC) and the lateral hypothalamus (LH), which may impact their ability to control or regulate emotional responses when anticipating rewarding meals or treats.
The dlHPC is located in the region of the brain that processes memory and the LH is in the region of the brain that is responsible for keeping the body in a stable state – homeostasis.
In the study, researchers were able to evaluate patients whose brains were already being monitored electrically in an epilepsy monitoring unit.
The team monitored brain activity as patients anticipated – and then received – a sweet treat (a chocolate milkshake).
Results showed that both the dlHPC and the LH activated simultaneously when participants anticipated receiving the rewarding meal. The dlHPC and LH also exhibited extremely strong connectivity.
In individuals with obesity, researchers found that the impairment of this hypothalamus-hippocampus circuit was directly proportional to their BMI.
In addition, for participants with a high BMI, the connection was even more disturbed.
To further validate the connection, the research team used a technique called “brain clearing,” to analyse brain tissue.
The technique revealed melanin-concentrating hormone, a hormone known to regulate feeding behaviour that is produced in the LH. They found the presence of MCH in the dlHPC, and nowhere else, confirming a link between the two regions.
Previous research has found an association with loss of function in the human hippocampus in individuals with obesity and related disordered eating, such as BED.
However, outside of imaging techniques such as magnetic resonance imaging (MRI), the role of the hippocampus has been difficult to study in humans with obesity and related eating disorders.
Casey Halpern, associate professor of neurosurgery and one of the study authors, said: "These findings underscore that some individual’s brains can be fundamentally different in regions that increase the risk of obesity.
“Conditions such as disordered eating and obesity are a lot more complicated than simply managing self-control and eating healthier.
"What these individuals need is not more willpower, but the therapeutic equivalent of an electrician that can make right these connections inside their brain.
“The hippocampus has never been targeted to treat obesity, or the disordered eating that can sometimes cause obesity.
"We hope to be able to use this research to both identify which individuals who are likely to develop obesity later in life, and to develop novel therapies – both invasive and not – to help improve function of this critical circuit that seems to go awry in patients who are obese.”
To read the full research paper, click here for Nature
Close Window